The PC model(Pressure Cooker Model, PCM; van der Hulst, 2023) is a newer and clearer psychological model that uses everyday metaphors to describe the understanding of functional neurological impairment. It has been developed based on years of clinical experience in treating patients with all forms and subtypes of functional neurological disorder. The focus of the model is on intra-individual, inter-individual, cognitive, emotional and behavioural processes.
Layers of the model
-
Factors and history of key (psychological) events
Adverse childhood events (trauma, abuse, maltreatment)
Events that occurred closer to the onset of FND symptoms
-
Tightly closed lid (Reduced verbal expression of emotions) -
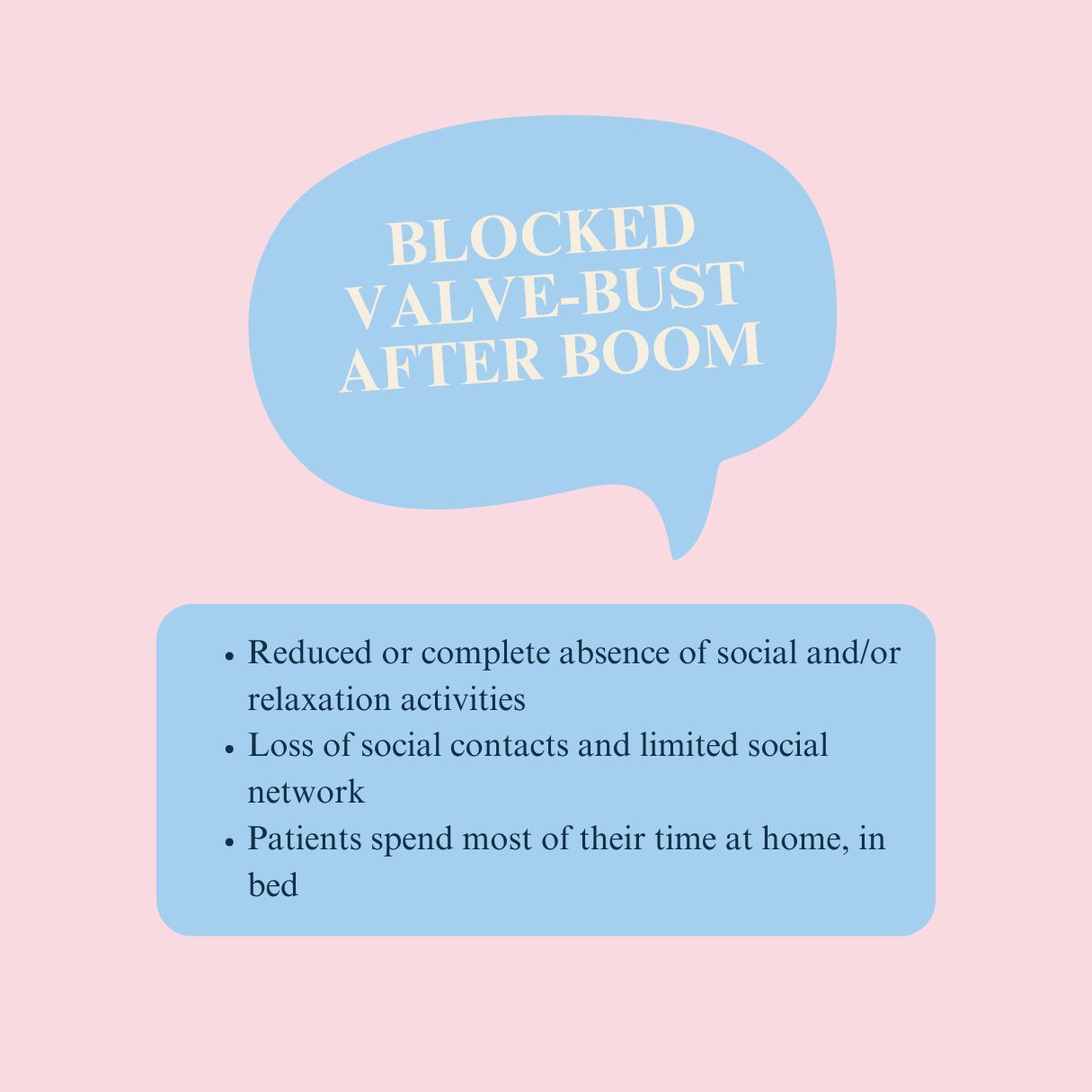
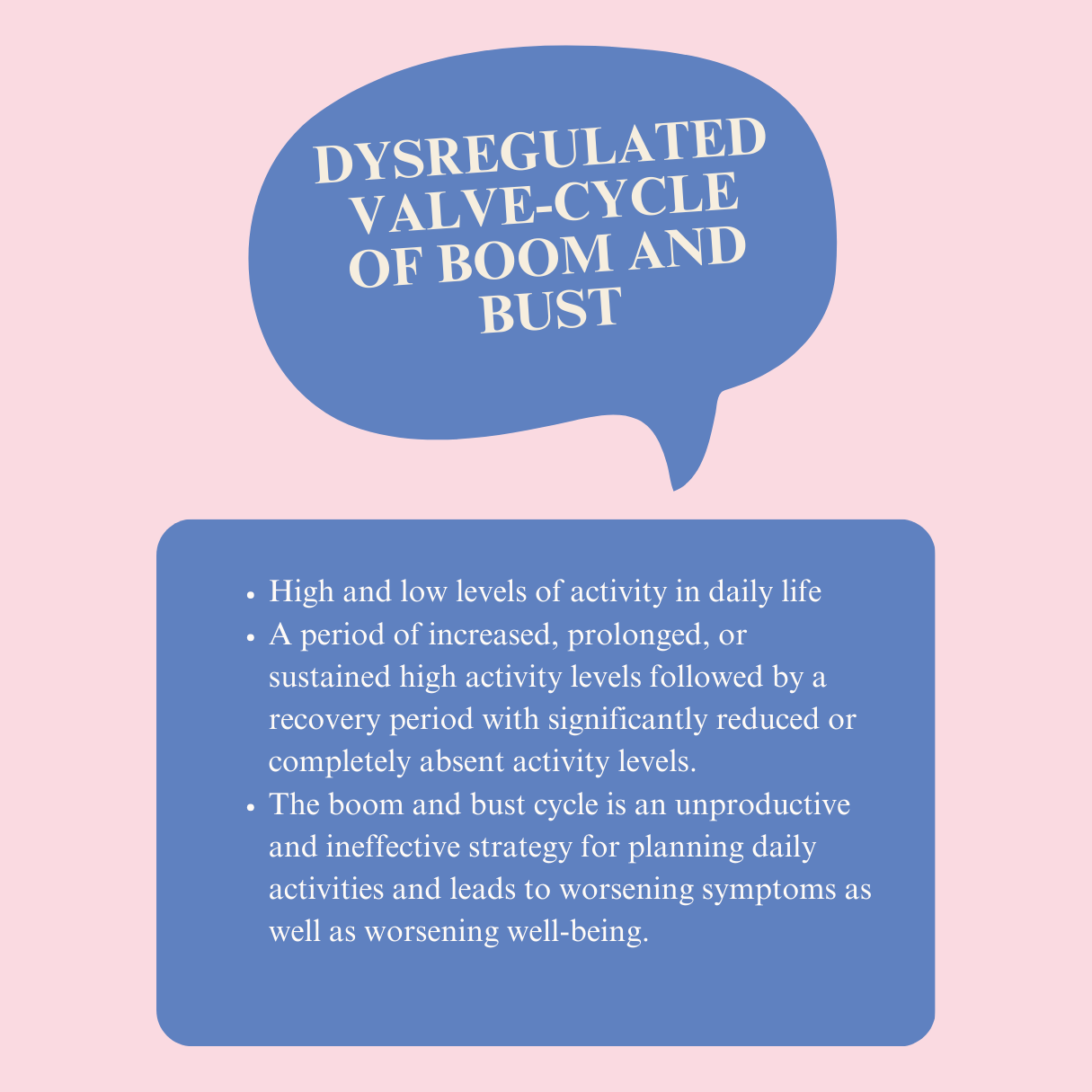
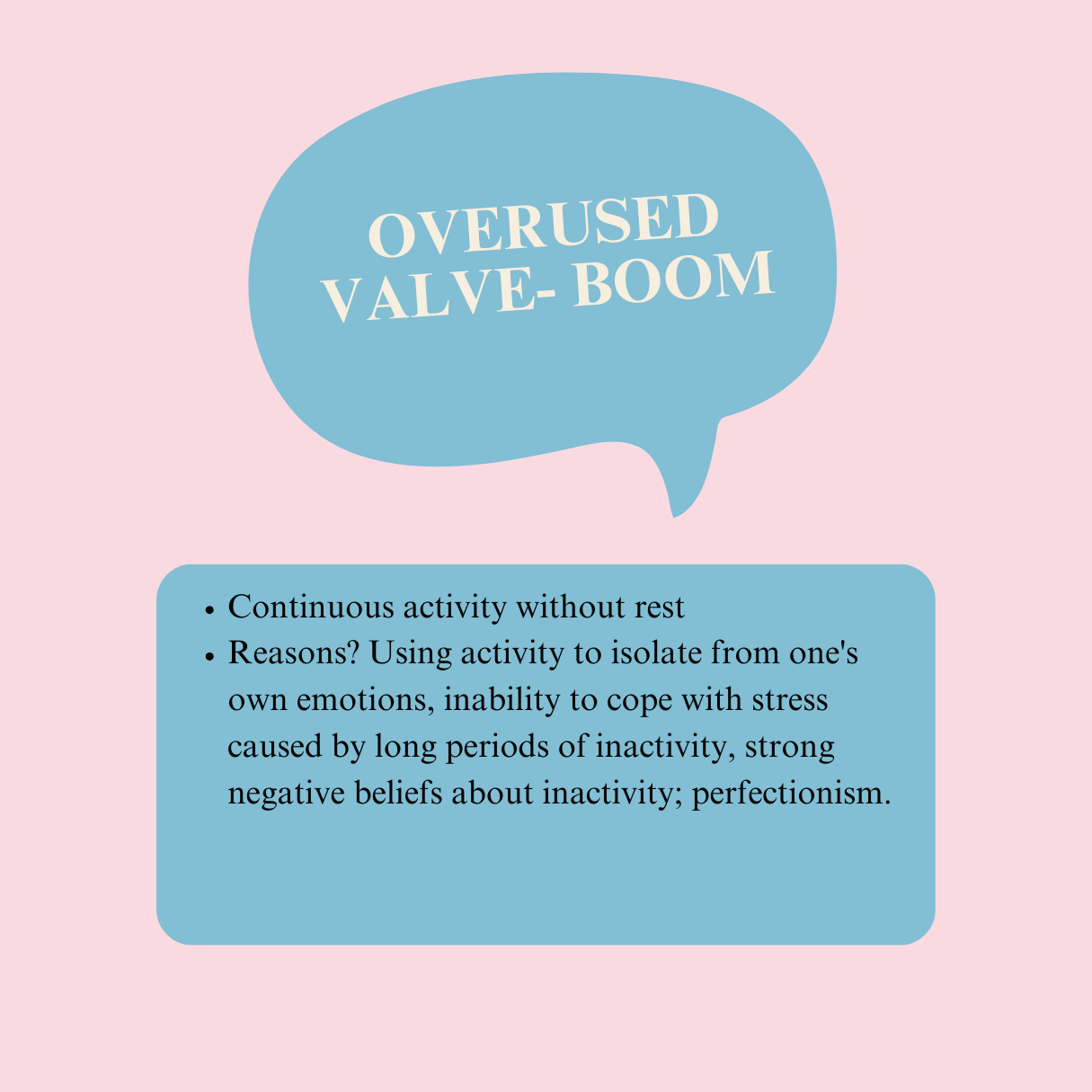
Blocked/disregulated/used steam valve (Abnormal activity levels)
Sticky food leftovers (Coping strategies from childhood that have carried over into adulthood)
Dissociation (A way of coping with difficult emotions)
-
Fuel (daily triggers, interactions or stressful events that stimulate FND symptoms)
Flames (Negative (automatic) thoughts, feelings or memories or ill-defined internal states that trigger FND symptoms)
Fever(Intensity of emotions in response to stressor(s))
Plug under too much pressure(Functional neurological disorder, pain, fatigue)
-
Potty (Acronym: FND SELF CARE = diet, sleep, medication, illness, aids, bladder function, fight or flight response, contacts, ability to take care of self, risks, physical activity, exercise and physical activity)
Warning light (Increased self-focus on symptoms)
-
Kitchen
System integration
family dynamics;
abnormal characteristics of relationships with health professionals;
amplification of interference on both sides;
Systemic re-tradmatisation;
prejudices/blind spots of professionals involved in the treatment of the disorder)
Ignition
Ignition represents the critical events or triggers that are most likely to have contributed to the development of a functional neurological disorder.
Profile 1: before-and-after
This profile is characterised by the development of FND following a critical event, which may be either a stressful or traumatic life event (e.g. divorce, accident, death, assault) or a previous illness and/or medical intervention (e.g. surgery). Traumatic childhood experiences and/or the development of inappropriate coping strategies are also common (but not necessary!) for this profile, as are negative interpersonal dynamics in the family at the time of the development of the first symptoms.
Profile 2: Sudden development
Some patients also report a sudden onset of panic attacks. This profile is strongly associated with anxiety manifestations and often results in non-epileptic or dissociative episodes.
Profile 3: Progressive development
Some patients are also characterised by a long period of various abusive behaviours (e.g. violence, toxic relationships) which may make them even more vulnerable to developing FND. On the other hand, there are also patients who experience stress (e.g. from work) for long periods of time in the absence of useful coping strategies and who, after a certain period of time, reach a point where the body reacts with illness.
Pot
The pot presents a number of physical and medical-contextual factors that maintain and/or influence FND, which can be remembered by the English acronym FND SELF CARE.
Nutrition
Check the content and frequency of the patient's diet
It is also a good idea to check how stress and emotions affect their eating
Gut health (If there are problems, refer to a specialist for a diagnosis of irritable bowel syndrome)
Weight (Does the patient have weight problems that affect the course of rehabilitation?)
Is the patient deficient in vitamins and minerals? (In individuals where social isolation is pronounced, vitamin D deficiency is possible)
Sleep
Check if the patient has an associated sleep disorder
Ask him about the quantity and quality of his sleep
Check all stages of sleep (preparing for sleep, falling asleep, waking in the early hours, hypersomnia)
Medications
Check the combination and dose of the medicines the patient is taking
Check if the patient's use of the medication represents a psychological safety behaviour (e.g. ending a dissociative episode with the medication)
Check that he is taking his medication correctly
Disease
Check the patient's medical history
Has he/she also been diagnosed with organic diseases such as epilepsy?
Use of aids
What tools does he use? What role do these devices play in the patient's life?
Is the patient's home adapted to the FND? How?
What is the psychological significance of assistive devices? Have they become part of his identity? Do they represent a form of safety behaviour?
Bladder and fluid functioning
Does the patient have any problems with urination, bladder or incontinence?
When it comes to fluids, be wary of drinking too much energy drinks, alcohol and caffeine.
Fight/flight and warning signs
Do you often feel stressed? Where in your body do you feel stress the most?
Look for objective signs of stress (e.g. difficulty sleeping, eating, lack of motivation, focus)
Notice any warning signs?
Contact
Ask if they ever call the on-call clinic for FND symptoms
Ask about past experiences with health professionals. Has the patient been a victim of systemic re-traumatisation?
Independence
Is the patient independent in daily activities? Does he/she need help anywhere?
Is the patient no longer doing an activity they used to enjoy?
Check family support. How have family roles changed? Check if there are any ways in which the family maintains the symptoms of FND.
Risk assessment
Risk of iatrogenic harm (wrong or excessive dose of medicines; excessive medical tests)
Physical symptoms (pain, fatigue, etc.)
Use of assistive devices as a safety behaviour
Unintentional self-harm (falls due to balance problems, problems assessing fitness)
Exercise, movement and physical activity
What is the patient's mobility? (e.g. balance)
Do you play any sports?
Have you had to give up any sport because of the FND?
Fuel
Fuel presents triggers that initiate FND episodes and/or exacerbate FND symptoms
Emotional triggers
Patients with FND may experience over-regulation of emotions, which can lead to avoidant behaviours, dissociation and suppression of emotional states, or a lack of emotion regulation.
Physical triggers
Patients diagnosed with psychogenic non-epileptic seizures often report physical triggers for dissociative seizures: heat, noise, intense light, pain, fatigue, etc.
Interpersonal triggers
Interpersonal triggers occur in the relationship between the patient diagnosed with FND, their symptoms and their social environment. They are often accompanied by feelings of guilt, shame and rejection (e.g. family quarrels, unmet need for belonging and affection, experience of lack of support).
Re-triggers
Re-triggers are a specific type of trigger, mainly experienced by patients with a history of childhood trauma. A mundane or even neutral stimulus can activate feelings associated with the trauma experienced.
No triggers
Sometimes patients report the absence of triggers, which can be extremely frustrating for both the patient and the clinical (neuro)psychologist/psychiatrist. Check if the cause is lack of awareness (e.g. alexithymia).
Flames
The flames represent aversive beliefs about the self, others, the world or the future. They also include emotional processing problems.
Beliefs about yourself
Self-image
Beliefs about the body
Beliefs about others
Negative social emotions ( shame, guilt, rejection)
Beliefs about interpersonal relationships
Beliefs about the world
Security
Psychological/physical threat
Beliefs about the future
Fear of recovery
Fear of relapse
Fear of new functional symptoms
Fear of falls
Heat
Heat represents the intensity of emotions. The heat can be adjusted on the pressure cooker. In the context of FND, we are talking about three settings.
Low setting = Dissociation
Dissociation in the context of FND is often triggered by intense emotions that are unbearable for the individual, both on a conscious and unconscious level. Dissociation is a defence mechanism through which the individual 'cuts off' all emotions to avoid confronting them.
High-low-high-low setting= Emotional deregulation
Rapid fluctuations between experiencing high-intensity and intense emotions and experiencing emptiness and numbness. This includes difficulties in naming and identifying emotions and difficulties in coping with and regulating emotions during stressful events, which affects interpersonal dynamics.
High-to-low setting
Characteristic mainly of functional seizures. Gradual development of a negative emotion, arousal or an unidentified internal state, leading to a climax, then gradually progressing to dissociation.
Sticky foods
Sticky foods represent ineffective coping strategies that we have internalised in childhood.
Cover
The cover represents the verbal expression of emotions.
Tightly closed cover
Reduced verbal expression of negative emotions in a psychologically safe and trusting relationship. Opening a tightly closed cover (verbalising and expressing difficult emotions that the patient has suppressed for a long time) often improves FND symptoms.
Valve
The valve represents abnormal activity levels.
Warning light
A warning light represents abnormal attention to physical symptoms.
Overload of physical symptoms
The patient is overwhelmed by physical symptoms, which are clearly expressed in his speech, cognition and behaviour. A large part of psychological therapy is devoted to talking about the physical symptoms. The patient minimises psychological factors and prefers physiological and organic reasons for the onset and maintenance of FND.
Hypervigilance
The patient hypervigilantly monitors FND symptoms, body functions and sensations. Systemic hypervigilance can also occur, where family members are abnormally attentive to physical symptoms and warning signs, leading to either a worsening of symptoms or a dissociative episode, which amplifies the patient's abnormal attention. Hypervigilance may also be triggered by devices in the patient's environment if they represent protective behaviours.
Identity
The patient's identity is defined by a functional neurological disorder.
Overpressured plug
A plug that is under too much pressure represents the symptoms of FND and the pain and fatigue that result from FND
Kitchen
The kitchen represents the social function of the FND
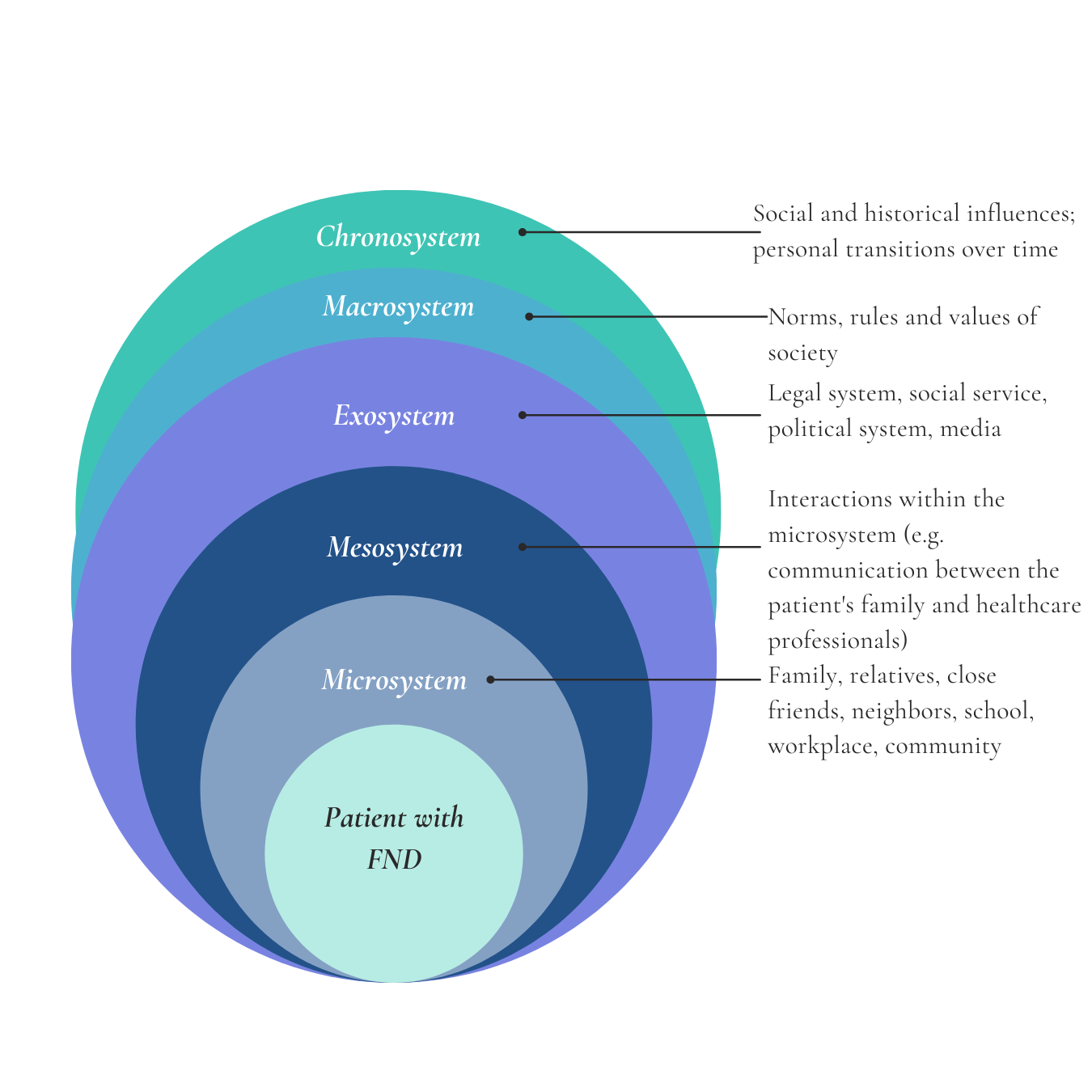
Bronfenbrenner's ecological system model
The Kitchen represents the external regulatory function of a functional neurological disorder and explores the influence of the social environment and interpersonal relationships, with the aim of identifying factors that potentially maintain and trigger FND symptoms. The PC model assumes a dynamic interaction between the FND diagnosed individual and the environment, the product of which is emotional deregulation that serves to establish psychological safety for both the patient and the environment. Based on modern research and clinical work, it is assumed that FND is maintained by biological, psychological and social factors. The complex interaction between the individual and the environment can also be explained using Bronfenbrenner's ecological system model.
Ecological theory illustrates the intricate interplay between the social environment and the individual, suggesting that understanding the connection between them can elucidate dysfunctional behavior and relationships. This model encompasses various social systems that reflect the varying levels of direct interaction an individual has with the environment.
Explaining the psychologist's perception of the treatment of FND patients using the PC model
-
Insisting on a psychological formulation reduces the psychologist's anxiety about his or her abilities
-
E.g. a clinical psychologist rarely or never sees a patient with FND
-
Clinical psychologists have been working with FND patients for some time, but the resistance to psychology is becoming more pronounced, the patient is very focused on his symptoms and insists on physical explanations only.
-
Fear of failure, frustration, low work self-esteem. "They'll think I'm not a good enough clinical psychologist!"
Vročina: high levels of situational stress
-
Childhood coping strategies, "I'm not good enough!"
-
E.g. sleepless nights
-
Excessive focus on resistance to psychological treatment and attempts to convince the patient that psychological treatment is important
-
Avoiding talking about resistance to avoid losing the patient
Boom and Boost cycle: feeling tired after treatment; no planning for other patients that day
-
Resistance to patient resistance: insisting on a psychological formulation
Explanation of the patient's resistance to psychology using a PC model
-
A clinical psychologist meets an FND patient For the first time and notices a reluctance to psychology and an increased focus on symptoms.
-
E.g. emotional neglect in childhood, parental figure never believed the patient, emotions were not talked about and/or expressed
-
E.g. referral for psychological treatment
-
"They think it's all in my head!"
-
Coping strategies from childhood, suppression of emotions, dissociation
-
E.g. unpleasant physical symptoms such as heart palpitations, hyperventilation, feeling dizzy
-
Excessive focus on FND symptoms
-
Lack of a safe relationship in which the patient can verbally express his/her feelings.
Blocked valve: social isolation, inability to test beliefs about psychology with others
-
Neglect of psychological factors, which is maintained by the FND