Acceptance and Commitment Therapy( ACT) is a psychological therapy based on Relational Frame Theory, which assumes that human language and thought is something we have learned to understand and generate, based on responses from our environment. People thus equate the construction of verbal language with events and live beyond the language they use to describe their lives(e.g. negative predictions about the future or guilt about the past), which makes them less in touch with the present moment. As a result, they respond more to verbal descriptions of events than to actual experiences, leading to emotional distress and psychological inflexibility. ACT is also based on functional contextualism, within which every behaviour, within a given context, has a function (Cope et al., 2017).
ACT has an effect on a transdiagnostic process called psychological flexibility, which consists of three components:
Ability to persist in or change behaviour in a way that involves a conscious and open attitude towards thoughts and feelings = Openness
Ability to appreciate what a given situation allows = Awareness
Ability to align behaviour with one's own goals and values = Engagement
ACT'S SIX CORE CONCEPTS
-
The present moment
ACT guides people to experience the present moment in the here and now.
Many activities require a degree of awareness in the present moment, but 'staying' in the present moment in the absence of an immediate threat or crisis is very difficult.
Creating greater awareness of experience helps to identify problematic patterns of behaviour or responses to external stimuli that would otherwise go unnoticed.
It allows for greater flexibility in responding, potentially leading to behaviour that is more in line with one's own values.
-
Values
Values are individual and unique standards that guide us in how to live a life that is personally meaningful to us. From this perspective, there are no wrong or right values, but we need to be aware that as we evolve and change, so do our values.
Based on this concept, it is evaluated whether the behaviour expressed by the client is closer or further away from his/her values.
-
Appropriate behaviour
Engaging in activities that are consistent with our values.
Sometimes engaging in activities that are in line with the client's values leads to a heightened sense of unpleasant inner experiences.
Still: the function is on behaviour, not on avoiding negative inner experiences.
Applying behavioural strategies from CBT, such as goal setting, exposure and skill acquisition.
-
Self as context
It is a unique way of experiencing oneself as separate from one's private mental experiences (thoughts, feelings, sensations). So, as a stable entity.
The person is an observer of his or her own experience, not the experience itself. In this context, it is the experience that changes, not the self.
-
Defusion
The cognitive component, which focuses on the perception of thoughts, emotions, memories; the response to them and the consequence of that response.
If we get so caught up in our thoughts and other personal experiences that we believe they are actually real, we are likely to react to them automatically and consequently try to avoid the situation.
In defusion, we experience our private events, but we have the opportunity to stop, step back and realise that a negative thought is nothing more than a thought.
The fusion of the self with thoughts thus leads to suffering. The patient learns to distance himself from unpleasant thoughts, such as "I will neverheal myself", which allows him to have more control over his own behaviour.
-
Acceptance
Practising and encouraging open acceptance of private events (thoughts, feelings, emotions, memories).
A willingness to get in touch with one's whole experience, including the unpleasant things that come up.
Process function: what causes us pain directs us to what is important to us.
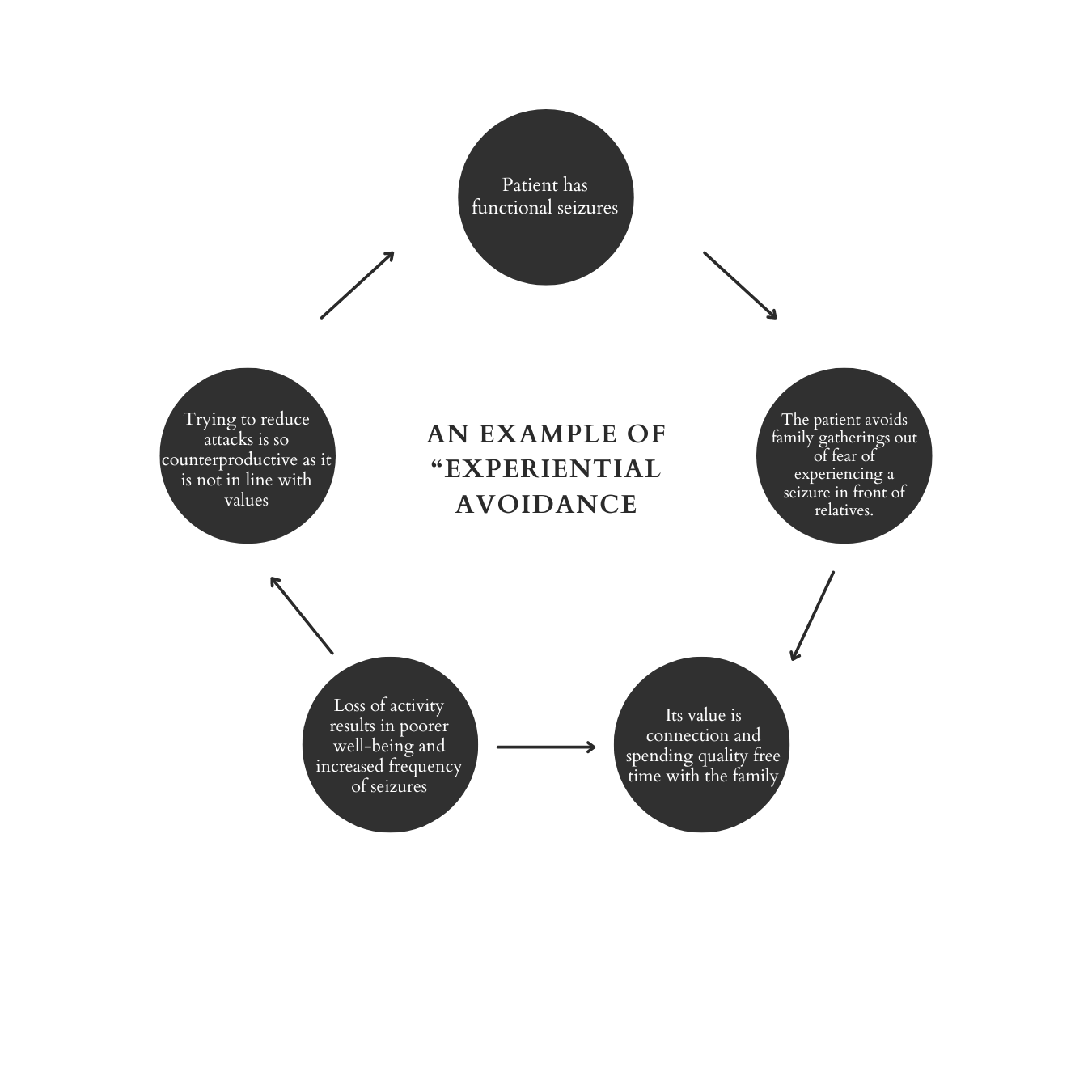
Psychological inflexibility refers to behaviour that is not controlled by chosen values or contigencies but by external experiences. This leads to so-called "experiential avoidance", whereby avoidance is used to avoid unpleasant internal experiences such as painful thoughts or feelings. This leads to emotional stress as the behaviour is not in line with one's own values.
Benefits of ACT for FND patients
Mindfulness and acceptance of the present moment
Increasing value-oriented behaviours
Examples of ACT techniques in the context of the FND (Graham et al., 2018)
-
Example of a functional analysis:
Behaviour: worry or rumination because no one believes FND symptoms are real
Antecedent: patient notices that symptoms have worsened
Consequence: excessive attention to symptoms
Function: confirmation that FND symptoms are real / correct prognosis of symptoms
Contingency: in the past, problem solving was negatively reinforced by reducing unpleasant feelings (e.g. in relationships or at work) and positively reinforced by achievement (e.g. through work, school, parental approval).
Clinical discussion:
"These painful thoughts and feelings often seem to weigh you down... as if unwanted guests have taken up residence in your house..." "What happens when you are overwhelmed by such thoughts and feelings? What do you do?"
Exercises:
Observing if the way you control or alleviate painful thoughts or feelings is consistent with value-driven behaviour.
Mindfulness techniques to help the patient practise coping with painful thoughts and emotions (in the initial stages, it is good to do this in a safe environment with a therapist).
-
Example of a functional analysis:
Behaviour: avoidance of an important social (family) event
Antecedent: fear and thoughts about what other people will think about how I walk / have expressed FND symptoms are present at the time of invitation
Result: less anxiety and thoughts about yourself as a person with FND
Function: experiential avoidance of anxiety and thoughts relating to altered identity (person with FND)
Contingency: negative reinforcement through anxiety reduction
Clinical discussion:
"Which activities make you happiest and which make you least happy?... When do you feel most alive?..." "Was this behaviour a step forward or a step back from what is important to you? What do you want your life to look like in five years?"
Exercises:
90th birthday party - ask patients to imagine their own 90th birthday party and think about what they would like to say about their life.
Finding out if their behaviour is consistent with their values - writing and researching the different values they have and how they fit with their behaviour. Try to identify the smallest step that will make their behaviour a little more aligned with their values next time.
-
Example of a functional analysis:
Behaviour: dissociation
Antecedent: experiencing a stimulus associated with stressful (traumatic) childhood experiences
Result: less presence and awareness of the present moment
Function: learned safety behaviours and experiential avoidance of current unwanted memories and emotions
Contingency: negatively reinforced through the avoidance method of reliving painful memories and emotions
Clinical discussion:
"Can you observe your current thoughts/feelings/opportunities?... Notice that your feelings and thoughts are like clouds? They come and go..." "If an older version of you walked into the room right now - what would you see?"
Exercises:
Notice who the observer is - a mindfulness technique that allows us to observe our thoughts and feelings
Mindfulness - mindful awareness of the present moment
Perspective-taking techniques: using deictic framing to 'view' a clinically relevant event from different perspectives (person, place and time).
Some concerns
-
There are very few studies confirming the effects of Acceptance and Commitment Therapy for the FND patient population. The problems lie in the small sample sizes, the heterogeneity of both the subtypes and the combination of core and associated symptoms expressed, and the individualisation of treatment for each patient. It would also be useful to conduct a future study comparing ACT with mindfulness-based therapies to see if the positive effects are due to mindfulness or value-based behavioural components. ACT is theorised to be particularly effective for the motor subtype of FND, as it is based on changing attitudes towards physical symptoms and shifting attention away from them, which should contribute to a reduction in their frequency and/or intensity.
-
There are studies that have found that some individuals may experience overwhelming emotions due to maintaining attention on them, which is a potential risk factor (Binda et al., 2022; Farb et al., 2010), but on the other hand, these studies have implemented more extensive and intensive mindfulness-based programmes, whereas ACT uses shorter and less intensive mindfulness strategies.
-
Acceptance and Commitment Therapy will require time and effort that some patients may not be willing and/or able to give. A broad assessment of the patient's condition, symptoms and possible comorbidities (e.g. depression, fatigue and pain, etc.) is important as these may affect outcomes. Like other behavioural therapies, touch therapy is based on behaviour change and, consequently, outcome and effectiveness are linked to behaviour change. It is worth considering an eclectic approach that combines techniques and strategies from different therapeutic modalities.
-
Binda, D. D., Greco, C. M., and Morone, N. E. (2022). What are adverse events in mindfulness meditation? Global advances in health and medicine, 11, 2164957X221096640.
Cope, S. R., Poole, N., and Agrawal, N. (2017). Treating functional non-epileptic attacks-Should we consider acceptance and commitment therapy?. Epilepsy & Behavior, 73, 197-203.
Farb, N. A., Anderson, A. K., Mayberg, H., Bean, J., McKeon, D., and Segal, Z. Emotion, 10(1), 25.
Graham, C. D., O'Hara, D. J., & Kemp, S. (2018). A case series of Acceptance and Commitment Therapy (ACT) for reducing symptom interference in functional neurological disorders. Clinical psychology & psychotherapy, 25(3), 489-496.
Gutkin, M., McLean, L., Brown, R., and Kanaan, R. A. (2021). Systematic review of psychotherapy for adults with functional neurological disorder. Journal of Neurology, Neurosurgery & Psychiatry, 92(1), 36-44.
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., and Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour research and therapy, 44(1), 1-25.