Treatment of children and adolescents
Over the last two decades, there has been a significant renaissance in the understanding, diagnosis and treatment of functional neurological disorders in children and adolescents. In this population, FND represent the complex interaction between body, mind and the social (family) context in which children and adolescents are embedded (Kozlowska and Mohammad, 2022).
The treatment of the population of children and adolescents diagnosed with FND has also in the past (and in some places still is) based on a lack of a broader and complex understanding of FND, which has led to stigma, rejection and lack of empathy on the part of health professionals (Kozlowska et al., 2021).
Some common problems experienced by children and adolescents and their parents (Kozlowska et al., 2021):
Belief that the child and/or adolescent is simulating symptoms
Failure to diagnose and provide appropriate explanations of the diagnosis
Immediate labelling of symptoms as purely psychological and rapid completion of the neurological examination
Suggesting that symptoms are the result of emotional/sexual/physical abuse without adequate evidence
Believing that no treatment will work
Belief that children and/or adolescents with 'real' symptoms are more deserving of treatment
Ridicule and negative public comments
These problems deepen the stigmatising culture that pervades functional neurological disorder, and the verbal and non-verbal communication of health professionals shapes the primary beliefs about FND held by children/adolescents and their parents, as the vast majority are hearing about it for the first time. Communication from health professionals can thus reassure them, give them a sense of security, being heard and accepted, or make them feel despair, stress and deepen their distress.
Therapeutic use of language - the first step towards healing
The use of child-friendly, therapeutic language and a safe psychological environment in which the child/young person feels emotionally accepted and secure is encouraged, allowing him/her to continue to grow emotionally.
The health professional tries to explain the diagnosis FND in a way that enables the child/young person to accept the diagnosis as well as to understand its mechanisms, factors and treatment plan. The health professional should always encourage the child/young person to stay healthy (Kozlowska et al., 2021).
The therapeutic use of language will not only strengthen the therapeutic relationship, but also the child's confidence in communication and respect, and his/her sense of understanding and acceptance.
How to explain neuroscience to a child?
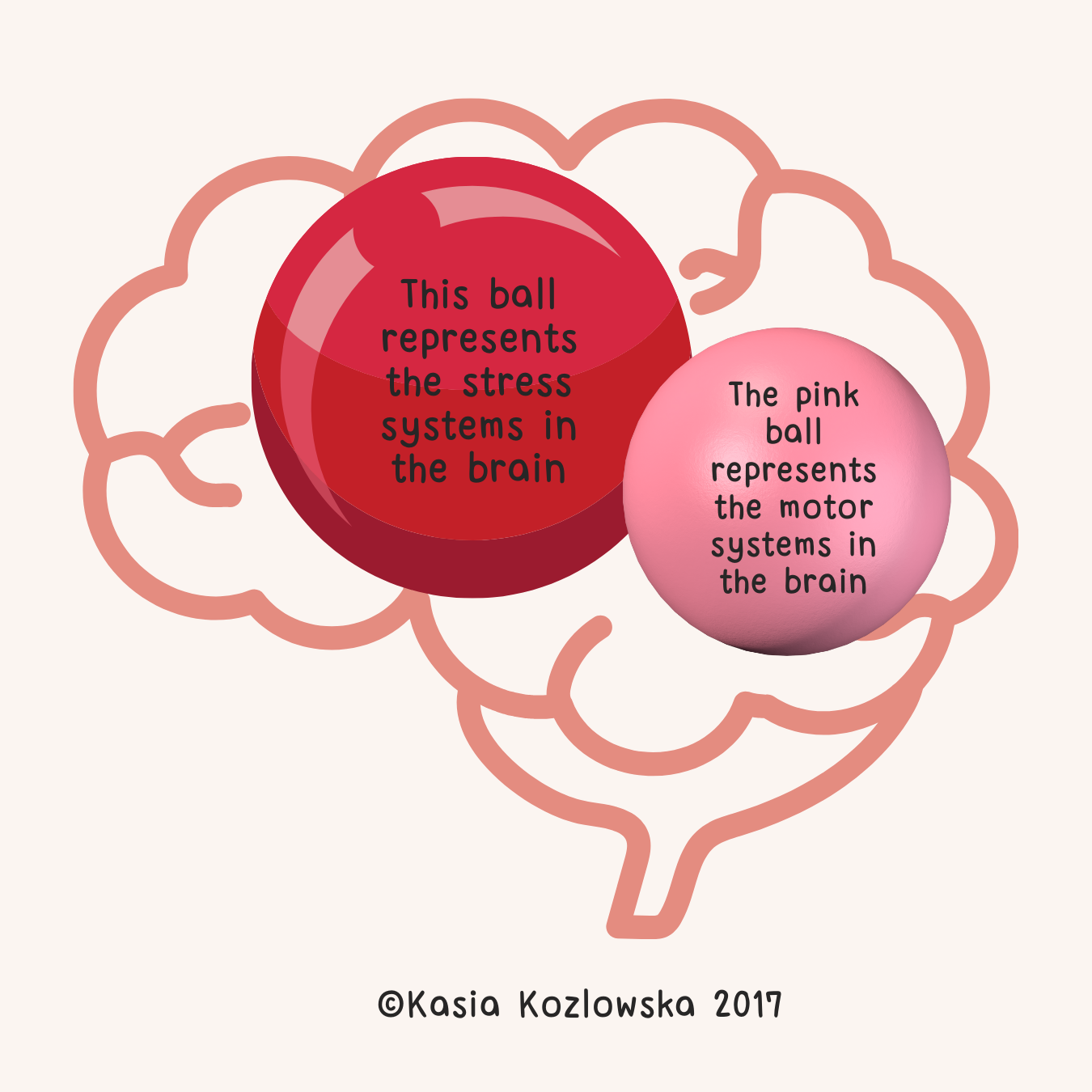
"The red ball represents the stress systems in the brain - the areas in the brain that are activated by stress. As this red ball starts to get bigger and stronger, it affects the pink ball, which represents the motor systems in the brain that are activated when you walk, run, ride a bike, etc. Physiotherapy will help you to strengthen the pink ball while we try to manage the growth of the red ball here. Once we have reduced the size of the red ball, your symptoms will most likely subside. Does that make sense to you?"
How to explain to a child what stress is?
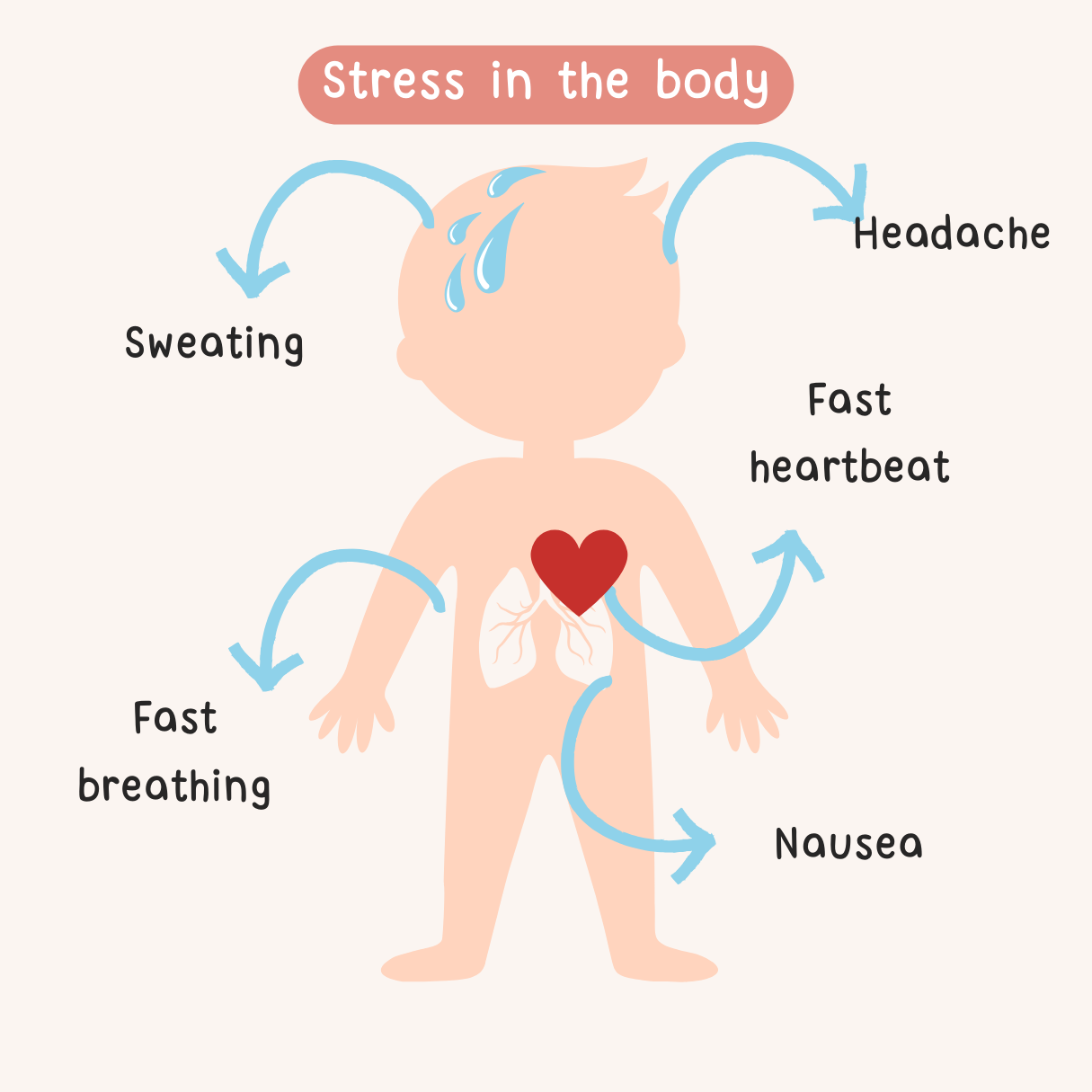
Explain to a child that the symptoms of red ball activation can be physical, emotional and behavioural. We give some examples of how stress manifests itself in the body:
Faster heartbeat
Faster and shallower breathing
Sweating
Headaches and abdominal pain
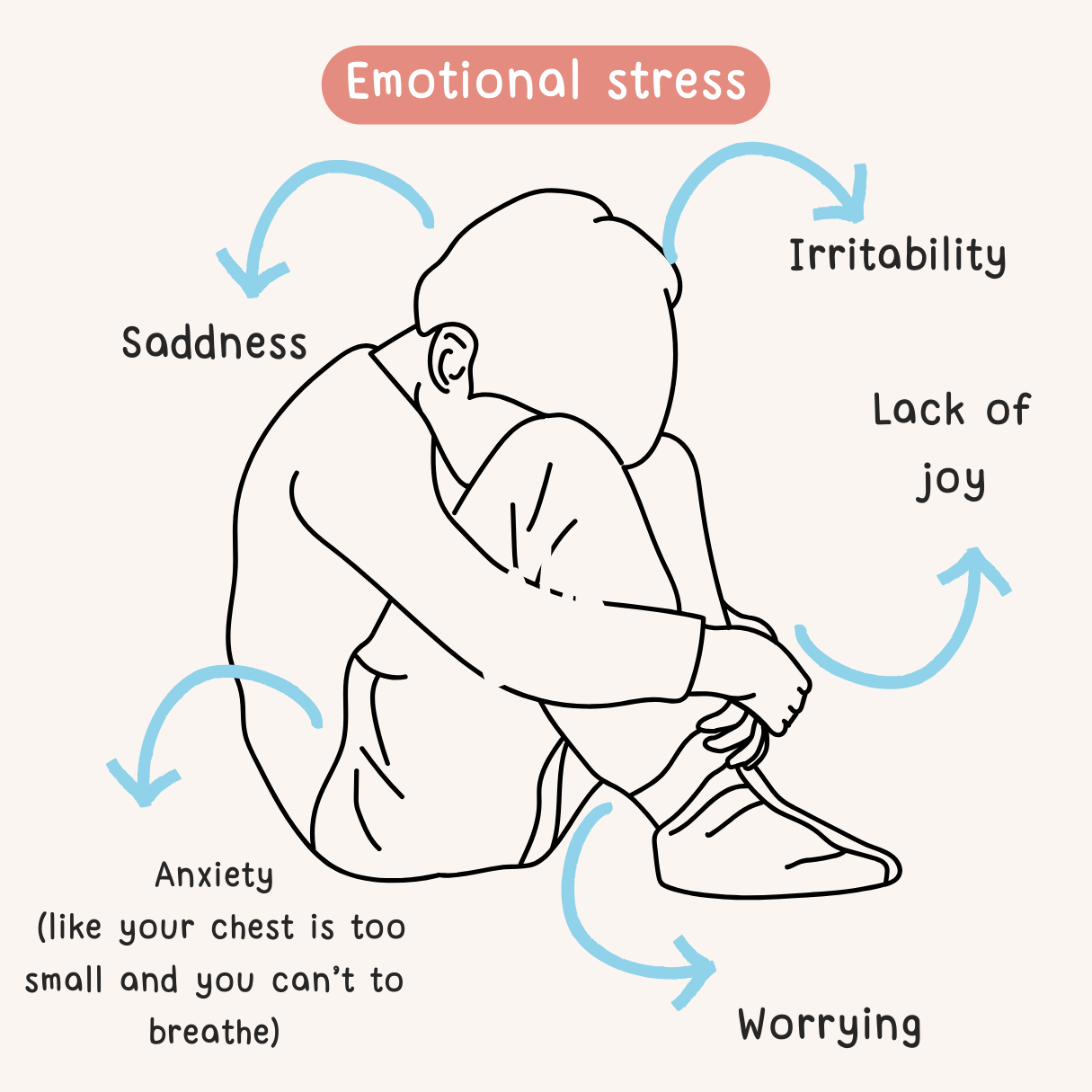
We also explain some examples of how stress affects our emotions and well-being:
Sadness
Anxiety
Fear
Irritability
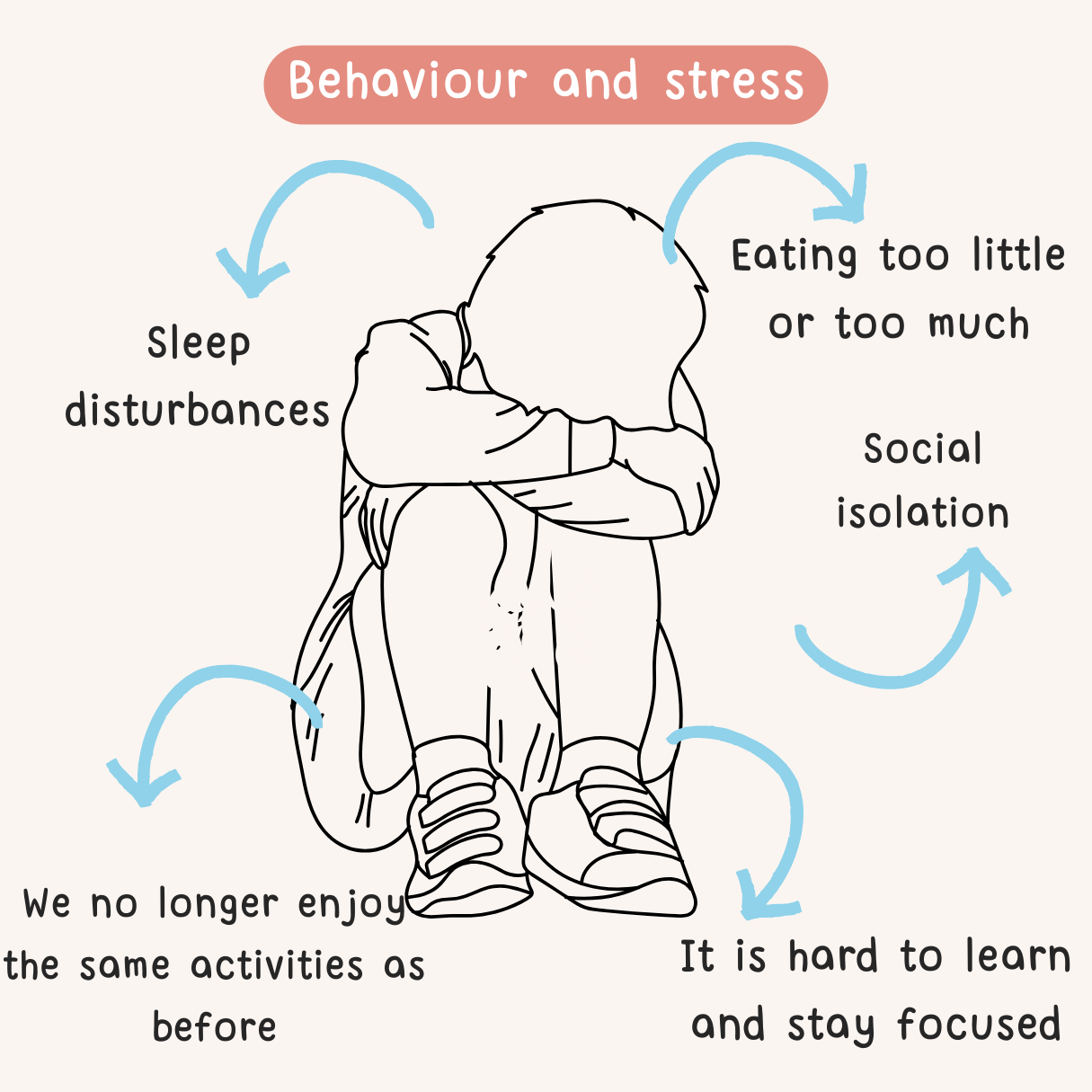
Finally, let's explain how stress affects our behaviour. We should be careful what words we use and not label behaviour as 'good' or 'bad'. This avoids giving the impression that the child is not 'good' because he/she is behaving in a certain way. Again, we explain that his behaviour is due to too many red balls in his brain and that together we will try to reduce them.
Treatment
As with adults with FND, treatment in children and adolescents is multidisciplinary.
-
Kozlowska, K., Scher, S., & Helgeland, H. (2020). Functional somatic symptoms in children and adolescents: A stress-system approach to assessment and treatment (p. 383). Springer Nature.
Kozlowska, K., Sawchuk, T., Waugh, J. L., Helgeland, H., Baker, J., Scher, S., in Fobian, A. D. (2021). Changing the culture of care for children and adolescents with functional neurological disorder. Epilepsy & behaviour reports, 16, 100486.
Kozlowska, K., and Mohammad, S. (2023). Functional Neurological Disorder in Children and Adolescents. In Symptom-Based Approach to Pediatric Neurology (pp. 699-724). Cham: Springer International Publishing.