Depression
We have all experienced changes in our wellbeing that have had a significant impact on our relationship with ourselves, others and the world. Fluctuations in how we feel are perfectly normal and act as signposts; they tell us that we need to change something to feel better. Clinical depression, on the other hand, manifests itself with symptoms that go beyond simple mood fluctuations. Thus, depressed patients report a loss of interest in activities and/or hobbies they once enjoyed, a loss of energy and appetite, feelings of sadness, hopelessness, irritability, lack of concentration and suicidal ideation, all of which have a profound impact on various aspects of their lives.
How common is depression?
Depression is one of the most common mental disorders, alongside anxiety, and statistics show that 25% of women and 12% of men will experience a major depressive episode in their lifetime.
Gender is thus a risk factor, but the underlying mechanisms are still not well understood.
Causes of depression
As with FND, causality in depression is determined by a combination of multiple factors. These may be biochemical, interpersonal, cognitive or behavioural.
Cognitive factors
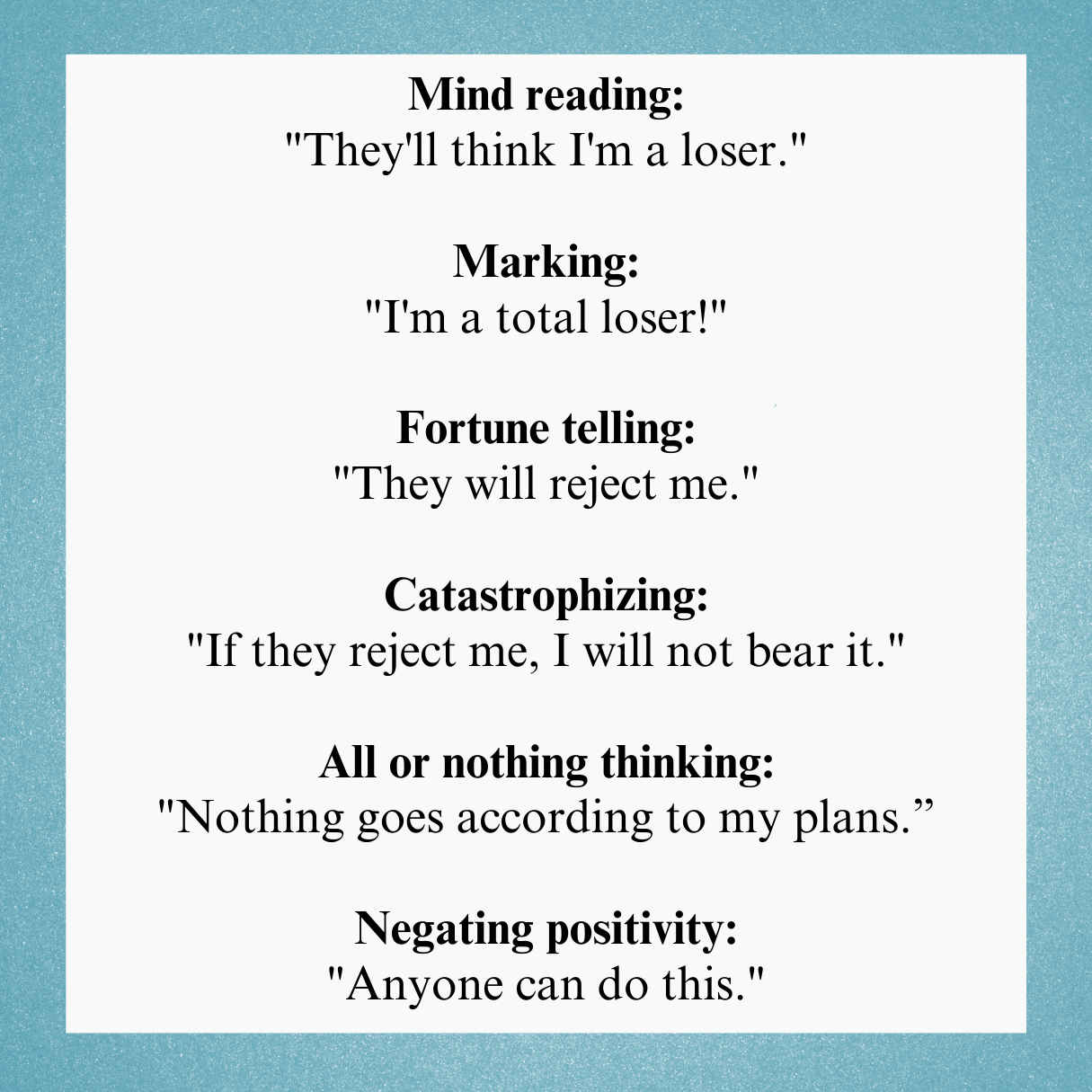
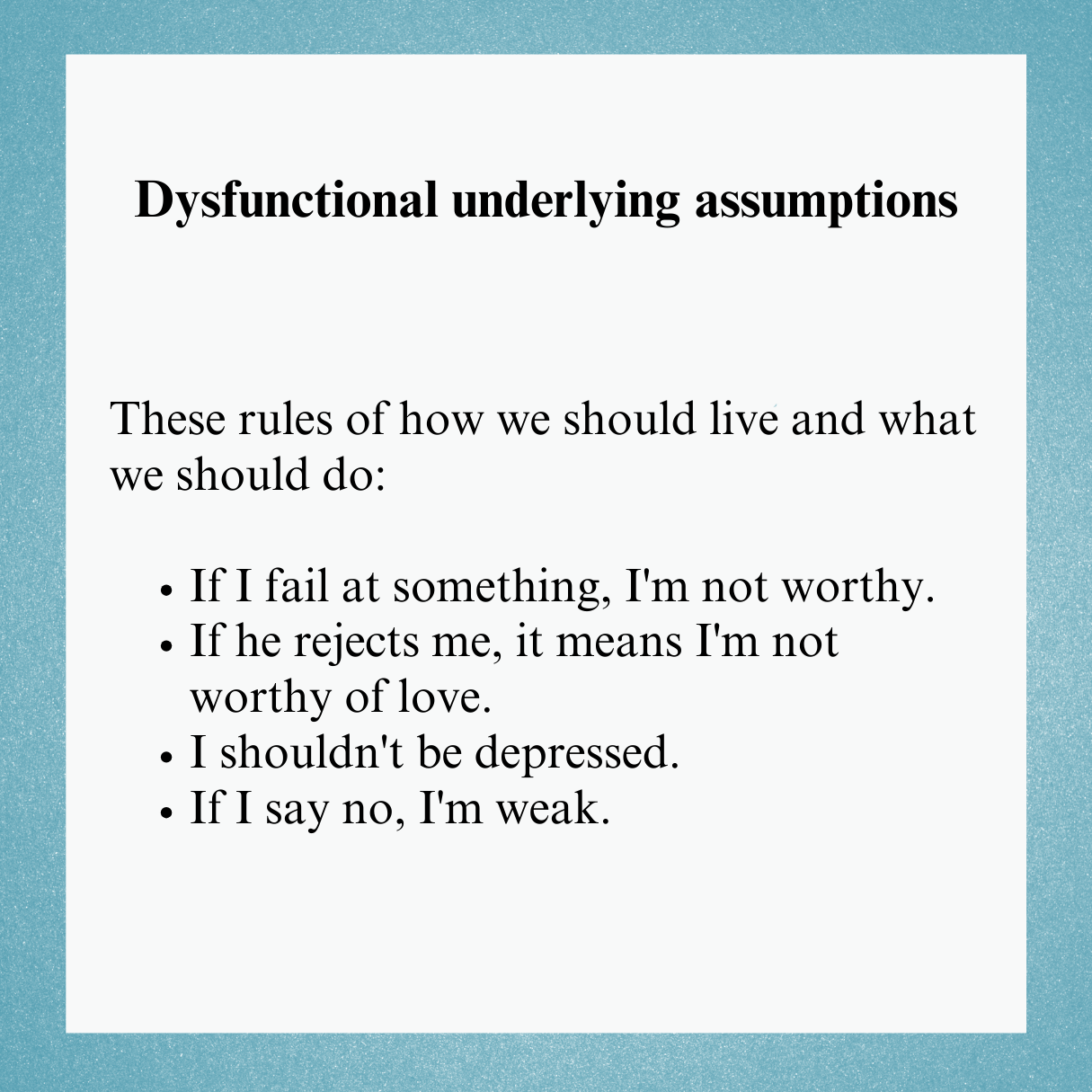
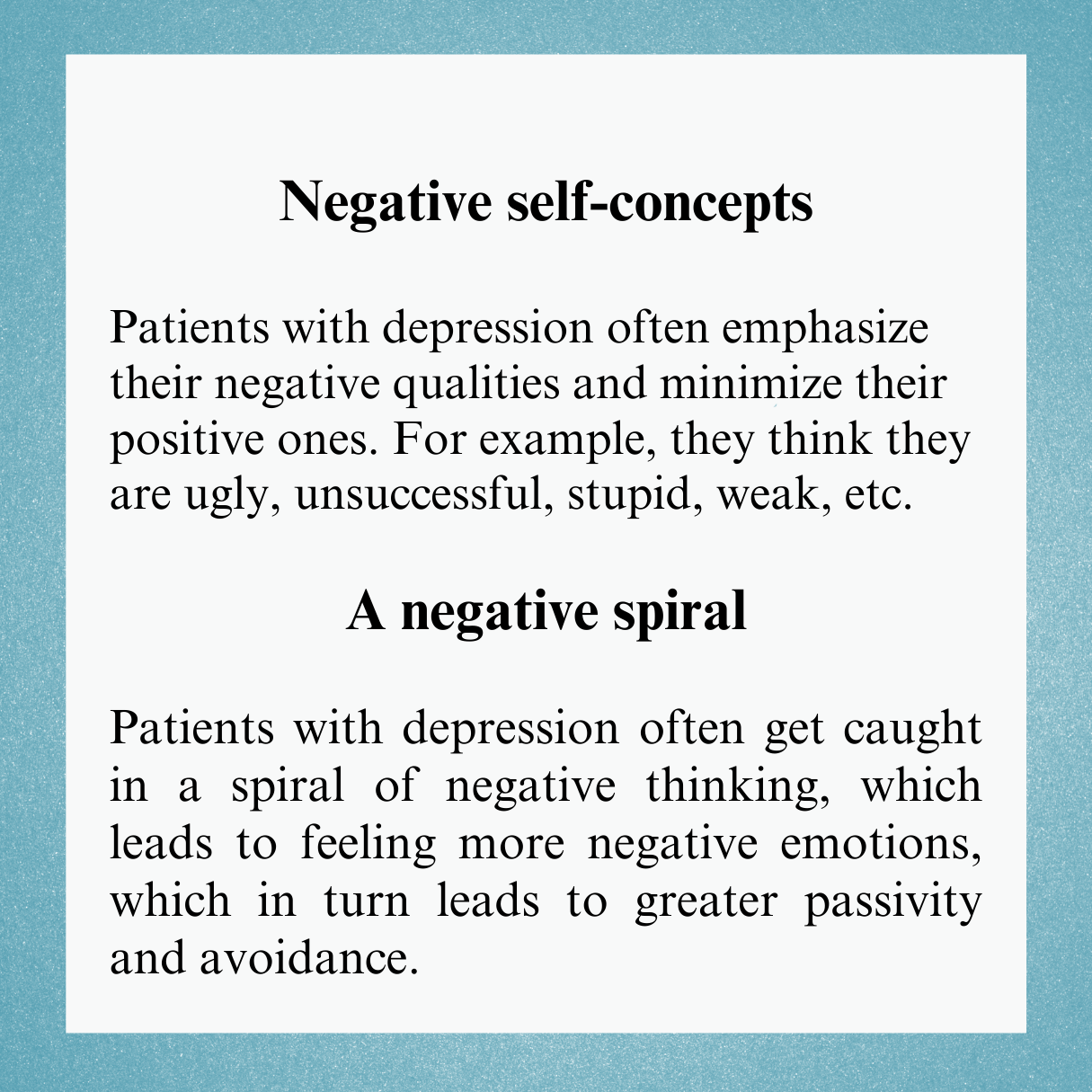
The way we think has a major impact on the symptoms of depression. There are four major maladaptive ways of thinking:
Negative automatic thoughts
Dysfunctional underlying assumptions
Negative self-concepts
Negative spiral of thought
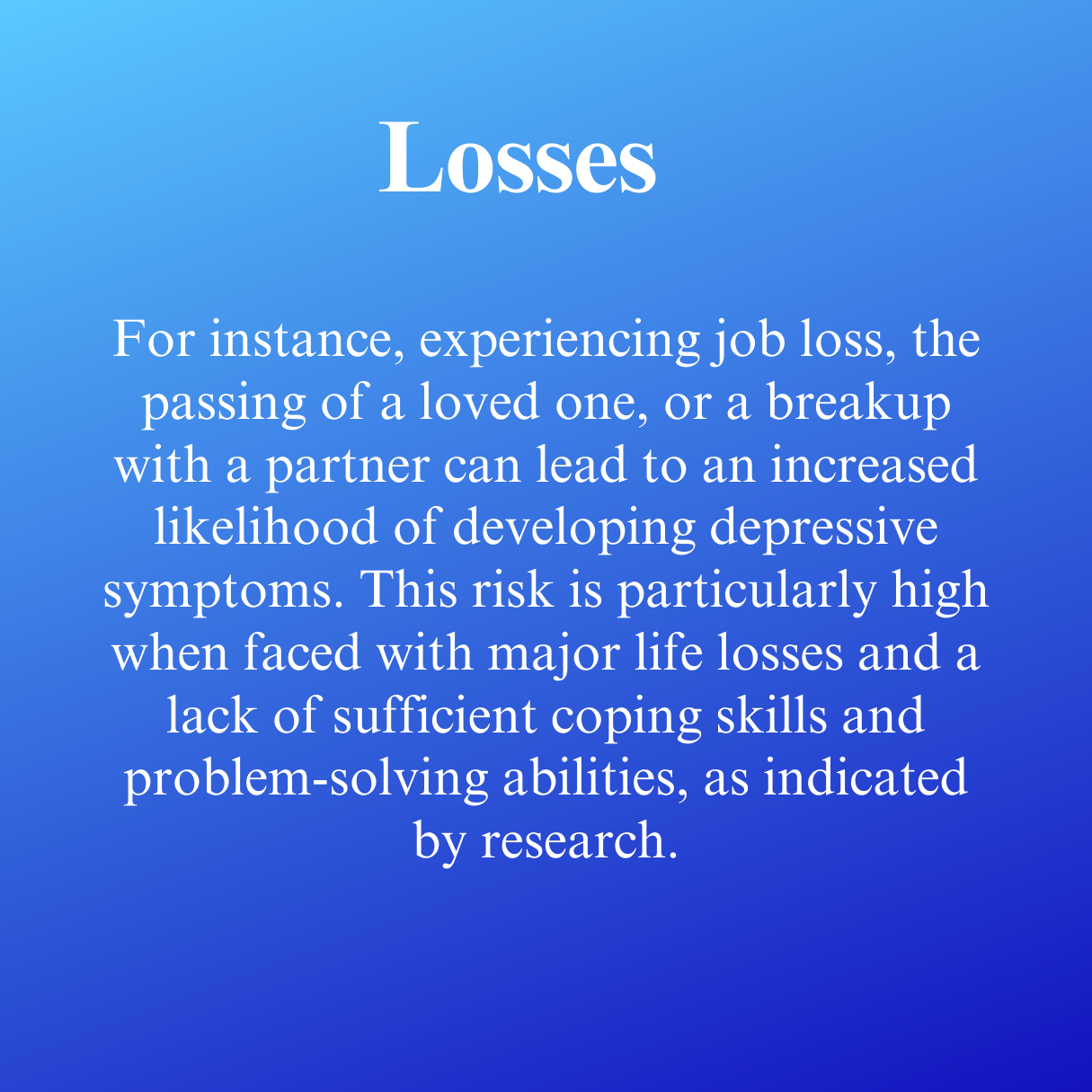
Behavioural factors are one of the multiple causes of depressive symptoms.
Although the factors described above can lead to the development of depressive symptoms, they do not necessarily result in depression. People may experience the loss of a loved one, but be skilled in 'coping strategies' such as refocusing attention, taking on new roles, increased levels of social interaction, rewarding behaviours, etc., which 'protect' them from developing the disorder.
Depression and FND
Experiencing depressive symptoms is common in patients with FND and is often the result of no one believing their symptoms. It is important to realise that experiencing depressive symptoms does not mean that you are 'weak' or that doctors will now assume that a mental disorder is the real cause of functional symptoms. Depression is often comorbid symptom and requires psychological management, as if inappropriately treated and managed it can exacerbate or even perpetuate functional symptoms. It is also important to note that depression can be diagnosed in the absence of depressed well-being. The criteria for the diagnosis of depression can be found below:
Five (or more) of the following symptoms have been present in the last two weeks and represent a significant change from previous functioning; at least one of the symptoms is (1) depressed mood or (2) loss of interest or pleasure.
depressed mood on a daily basis, either from a subjective report (e.g. I feel sad) or from a report from relatives (e.g. we hear her crying every day)
a marked decrease in interest or enjoyment in all or almost all activities during the day
Marked weight loss or gain; daily increase or decrease in appetite
daily insomnia or hypersomnia
psychomotor agitation or retardation (observed by others)
daily loss of fatigue or energy
daily feelings of worthlessness or excessive/inadequate guilt (guilt can be delusional; not just guilt about illness)
reduced ability to think or concentrate (either subjectively or objectively reported) almost every day
recurrent thoughts of death (not just fear of death), recurrent thoughts of suicide without a plan, attempted suicide or a specific plan for suicide
symptoms are not due to bipolar disorder
symptoms cause impairment in social, occupational and other important areas of functioning
the symptoms are not due to the direct physiological effects of substances such as drugs or medicines, or to a specific medical condition
grief does not explain symptoms better
-
Hölzel, L., Härter, M., Reese, C., in Kriston, L. (2011). Risk factors for chronic depression-a systematic review. Journal of affective disorders, 129(1-3), 1-13.
Leahy, R. L., Holland, S. J., in McGinn, L. K. (2011). Treatment plans and interventions for depression and anxiety disorders. Guilford press.
Pick, S., Anderson, D. G., Asadi-Pooya, A. A., Aybek, S., Baslet, G., Bloem, B. R., ... and Nicholson, T. R. (2020). Outcome measurement in functional neurological disorder: a systematic review and recommendations. Journal of Neurology, Neurosurgery & Psychiatry, 91(6), 638-649.