Functional seizures
Functional seizures are seizures similar to epilepsy, but with the difference that they are not caused by abnormal electrical activity in the brain, but by a process called dissociation. Dissociation is caused by a temporary change in the function (not the structure!) of the nervous system, which closely resembles a trance state.
There are mainly two types of functional (dissociative) seizures
With movements
Patients show movements that closely resemble a generalised seizure.
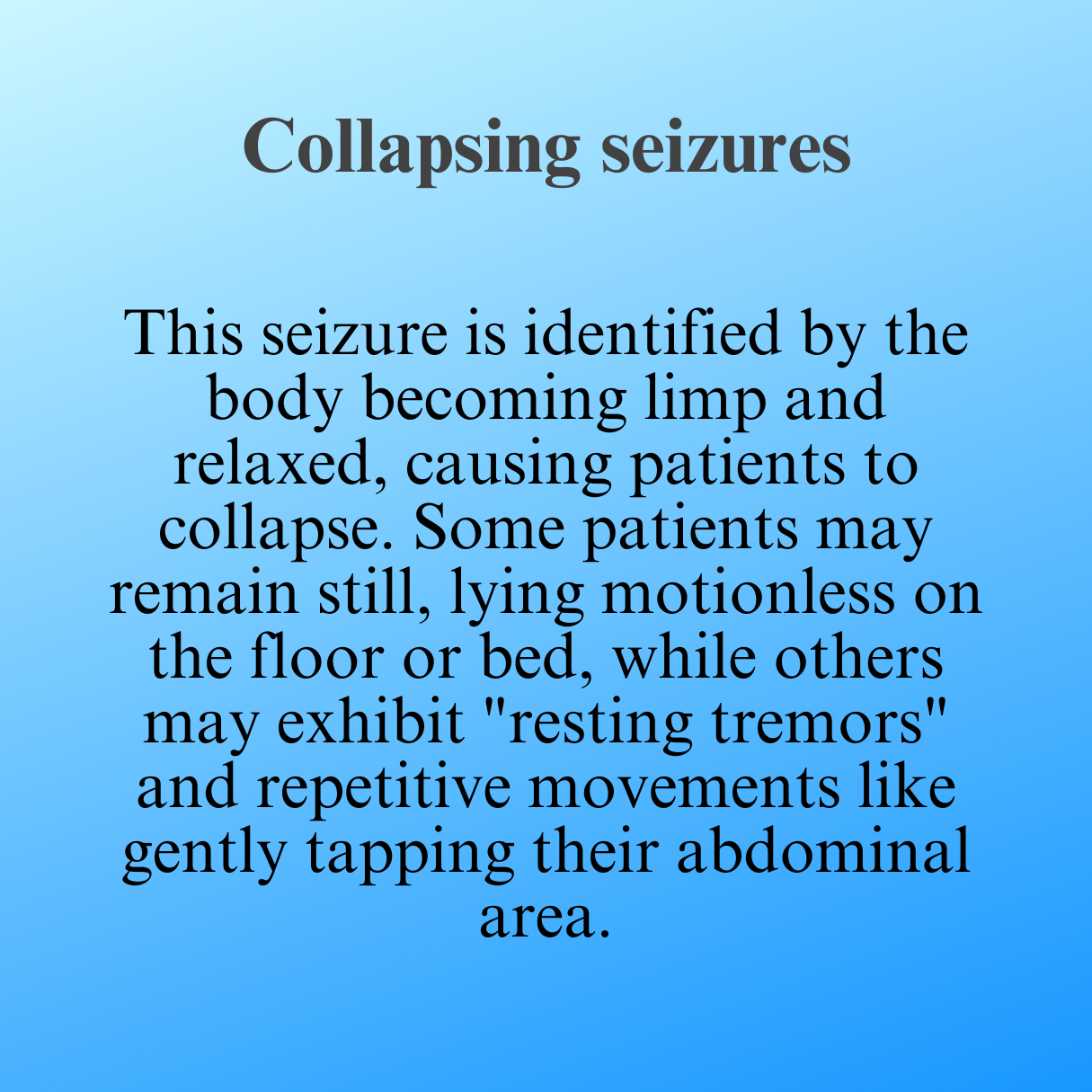
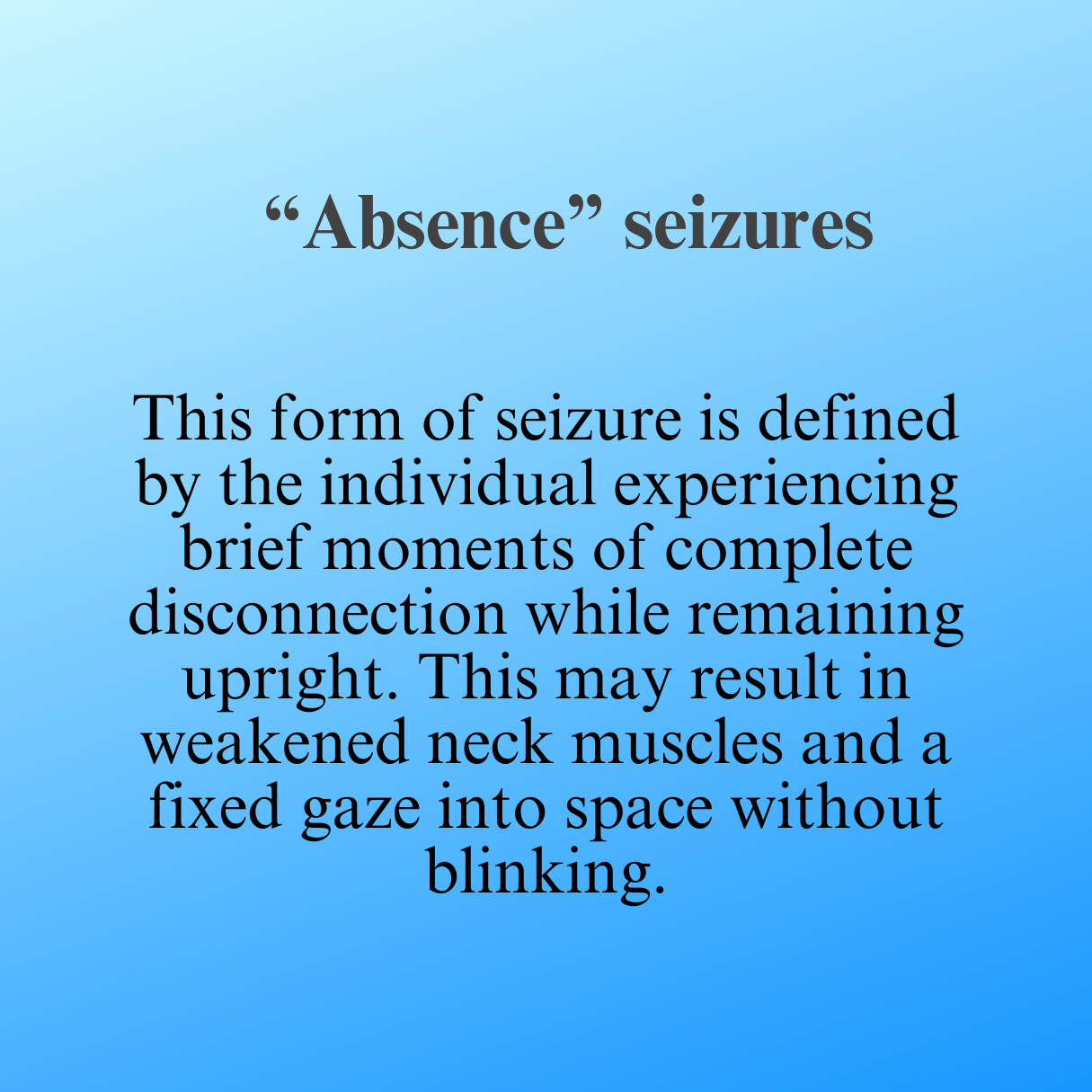
Without movements
Patients fall to the floor, where they lie motionless and unresponsive for several minutes. A period of intense staring is also possible.
Characteristics of functional attacks
Noticeable sudden paroxysmal change in behaviour or consciousness
Absence of electrophysiological brain characteristics characteristic of epileptic seizures (a combination of EEG and seizure videos is crucial for a correct diagnosis of functional seizures)
Absence of somatic causes of seizures (e.g. heart disease)
Seizures are usually time-limited and mimic epileptic seizures
Patients do not have voluntary control over seizures
Seizures are triggered by a range of psychogenic processes
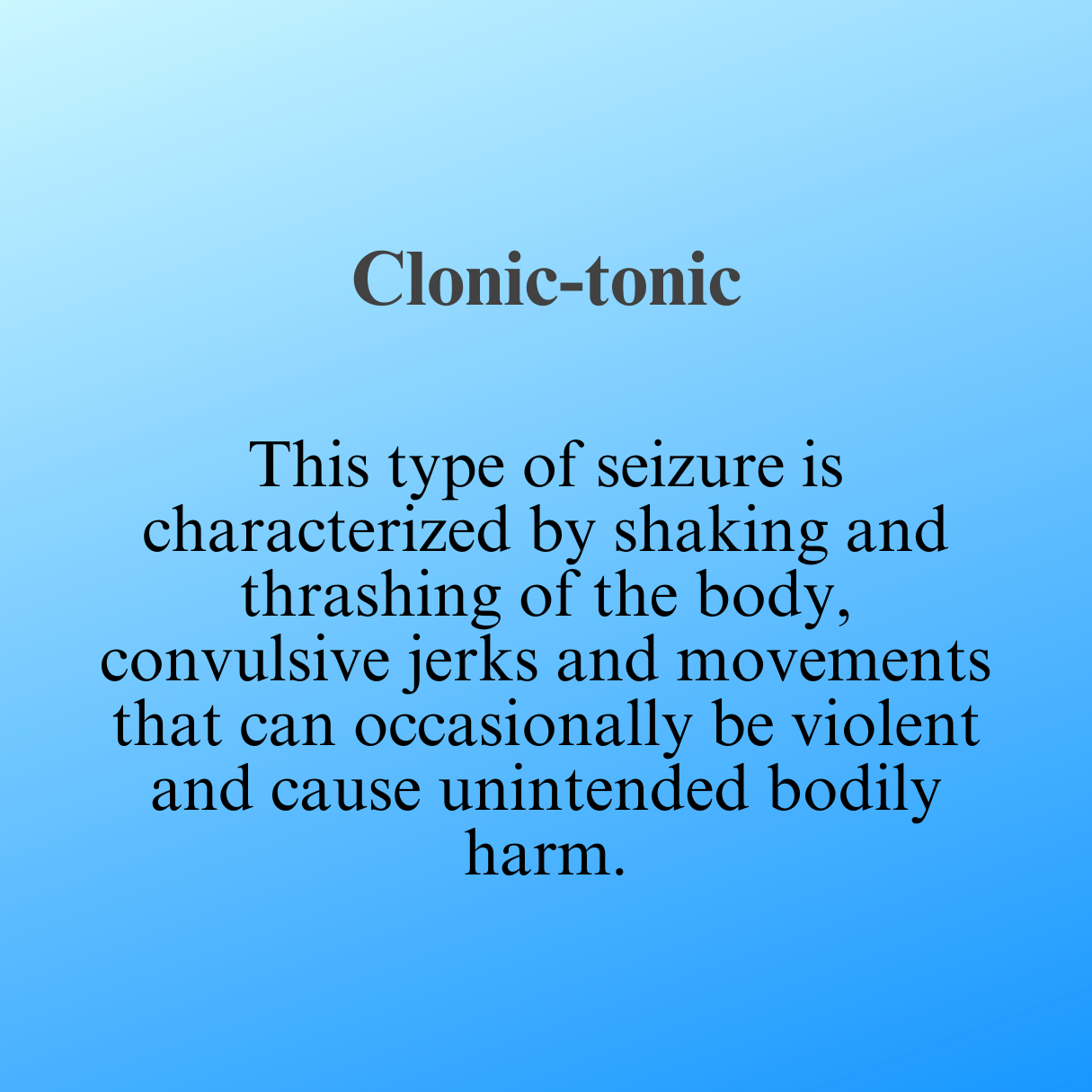
In more specific terms, there are three subtypes of functional (dissociative) seizures:
Key points
-
The diagnosis of functional seizures is one of the three most common diagnoses with temporary loss of consciousness and is diagnosed in approximately one in five patients experiencing seizures (Stone, 2008)
-
The diagnosis is more common in the female sex.
-
The onset of symptoms most often occurs in late adolescence or early adulthood. There are cases diagnosed in childhood.
-
Depression (57-85%)
Anxiety disorders (11-50% of patients)
Somatic symptoms and associated pain syndromes (22-84%)
Dissociative disorders (22-91%)
PTSD (35%-49%)
Personality disorders (10-86%)
-
Bennett, K., Diamond, C., Hoeritzauer, I., Gardiner, P., McWhirter, L., Carson, A., and Stone, J. (2021). A practical review of functional neurological disorder (FND) for the general physician. Clinical Medicine, 21(1), 28.
Bodde, N. M. G., Brooks, J. L., Baker, G. A., Boon, P. A. J. M., Hendriksen, J. G. M., Mulder, O. G., in Aldenkamp, A. P. (2009). Psychogenic non-epileptic seizures-definition, etiology, treatment and prognostic issues: a critical review. Seizure, 18(8), 543-553.
Bodde, N. M., Brooks, J. L., Baker, G. A., Boon, P. A., Hendriksen, J. G., in Aldenkamp, A. P. (2009). Psychogenic non-epileptic seizures-diagnostic issues: a critical review. Clinical neurology and neurosurgery, 111(1), 1-9.
Brown, R. J., and Reuber, M. (2016). Psychological and psychiatric aspects of psychogenic non-epileptic seizures (PNES): a systematic review. Clinical Psychology Review, 45, 157-182.
Brown, R. J., and Reuber, M. (2016). Towards an integrative theory of psychogenic non-epileptic seizures (PNES). Clinical psychology review, 47, 55-70.
Devinsky, O., Gazzola, D., and LaFrance Jr, W. C. (2011). Differentiating between nonepileptic and epileptic seizures. Nature Reviews Neurology, 7(4), 210-220.
Perez, D. L., and LaFrance, W. C. (2016). Nonepileptic seizures: an updated review. CNS spectrums, 21(3), 239-246.
Stone, J. (2006). Dissociation: what is it and why is it important?. Practical Neurology, 6(5), 308-313.